Colon cancer is one of the most common and potentially deadly cancers. The colon is an organ that plays a crucial role in digestion, and maintaining its health is essential for long-term well-being.
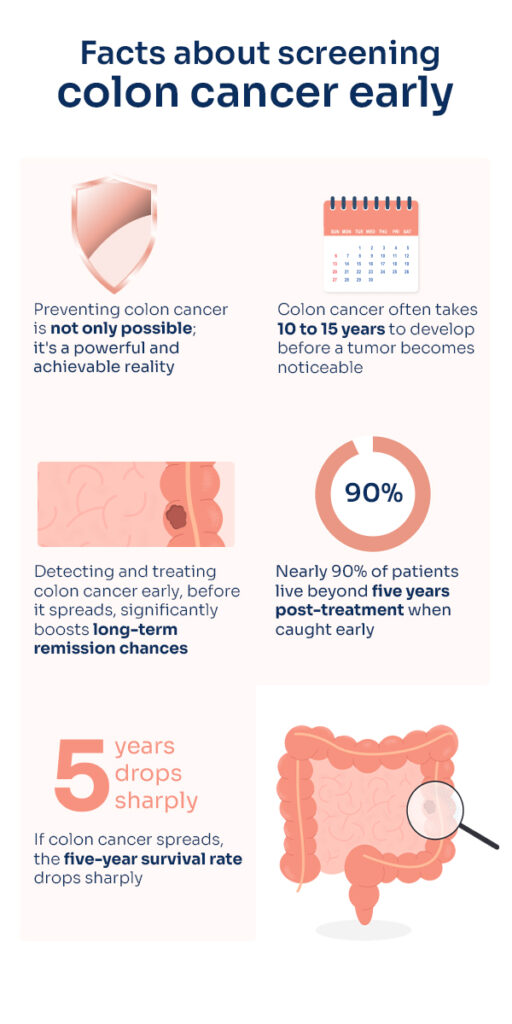
Preventing colon cancer isn’t just possible; it’s a strong and attainable reality. Early detection and treatment of colon cancer before it spreads to other organs significantly boost the chances of long-term remission. Nearly 90% of patients live beyond five years post-treatment when the cancer is caught early. However, if colon cancer spreads, the five-year survival rate drops sharply.
Colon cancer takes a long time to develop, often 10 to 15 years before a tumor is noticeable. Regular screening tests are thus vital tools in the fight against colon cancer.
By identifying and addressing potential issues early, you can enhance your chances of long-term remission and equip yourself with the knowledge to make informed health decisions.
This blog post will present compelling statistics highlighting the widespread nature of colon cancer and the crucial benefits of early detection.
How does colon cancer occur?
When normal cells in the colon undergo genetic mutations, they can lead to abnormal cell growth, resulting in tumors. These mutations can arise from various factors, including genetic predisposition, environmental influences, and lifestyle choices.
When these mutations disrupt the mechanisms that regulate cell growth, it causes an uncontrolled proliferation of abnormal cells, forming tumors in the colon. Multiple factors can contribute to these genetic mutations.
Genetic factors significantly impact the occurrence of colon cancer. Some individuals may inherit gene mutations that increase their risk. The gut microbiome and inflammatory processes within the colon can also significantly affect colon cancer development. Also, lifestyle choices, such as diet, physical activity, and smoking, play a role in this disease’s onset.
Colonoscopy is one of the primary and most thorough methods for screening for colon cancer. This procedure allows for a direct visual examination of the entire colon and rectum, enabling the detection of abnormalities, polyps, and potential cancerous growths.
During a colonoscopy, a flexible tube with a small camera (colonoscope) is inserted into the colon. Unlike other screening methods that focus on specific indicators like blood or DNA markers, a colonoscopy provides a comprehensive view of the colon’s health.
One of the major benefits of a colonoscopy is its dual capability to detect and treat issues during the same procedure. If polyps (small, benign growths) are found, they can be removed immediately, reducing the risk of them becoming cancerous in the future.
Virtual colonoscopy:
Virtual colonoscopy, also known as CT colonography or VC, represents a significant advancement in colon cancer screening technology. It provides a non-invasive, highly detailed alternative to traditional colonoscopy.
VC employs advanced computed tomography (CT) scanning to generate three-dimensional images of the colon and rectum. This innovative method eliminates the need for a traditional colonoscope, making it a less invasive and more appealing option for individuals who might be hesitant or unable to undergo a conventional colonoscopy.
 Lab tests for colon cancer screening
Lab tests for colon cancer screening
Other than colonoscopy, there are laboratory tests for colon cancer screening, providing non-invasive and informative methods for early detection.
Fecal occult blood test (FOBT):
This test identifies hidden blood in stool samples. Microscopic blood, often not visible to the naked eye, can originate from abnormal growths or polyps in the colon.
A positive FOBT result doesn’t definitively diagnose cancer but necessitates further diagnostic procedures, often including a colonoscopy for a precise evaluation. FOBT is a cost-effective, non-invasive screening method. This makes it suitable for routine use, ensuring broad accessibility.
Fecal immunochemical test (FIT):
The FIT operates similarly to the FOBT but specifically targets human blood, reducing false positives from dietary sources or non-human blood. This test offers greater accuracy, making it a more reliable tool for routine screenings.
Stool DNA test:
This innovative test examines DNA markers in stool samples, looking for cell changes that may indicate colon cancer or precancerous conditions. It is typically used with other screening methods for a comprehensive assessment.
Blood tests for tumor markers:
Blood tests provide another approach to colon cancer screening, focusing on specific markers associated with cancer cells in the bloodstream. Elevated levels of these markers can indicate the presence of cancer, aiding in early detection.
For diagnosed colon cancer cases, monitoring tumor marker levels through blood tests is essential for treatment plans.
At RGCC, advanced circulating tumor cell (CTC) tests, such as Oncotrail and Oncotrace, are valuable for colon cancer patients. These tests detect the presence of CTCs in diagnosed patients.
The Oncotrace test helps establish a baseline at the beginning of treatment, while the Oncotrail test monitors treatment effectiveness.
These tests provide critical information on the efficacy of current treatments and assist in personalized treatment planning. Follow-up tests also help monitor health and assess recurrence risk.
Screening frequency for colorectal health
The recommended frequency for colorectal cancer screenings depends on your age, risk factors, and the specific screening methods used. Common guidelines include:
Fecal occult blood test (FOBT) and Fecal immunochemical test (FIT): Advised annually for individuals at average risk.
Stool DNA test: Typically suggested every three years, though this can vary based on individual risk factors.
Blood tests for tumor markers: The frequency is determined by individual risk factors and treatment plans for those diagnosed with cancer.
Colonoscopy: generally recommended every 10 years for average-risk individuals, with more frequent screenings for those at higher risk.
Virtual colonoscopy is often suggested every five years for those at average risk.
Individuals with a family history of colorectal cancer or other risk factors might need more frequent screenings or to begin screening at an earlier age.
Consulting healthcare professionals
Consulting with your clinician or healthcare professional is crucial to determining the most suitable screening options for you. They will perform personalized risk assessments, considering your age, family history, and personal health.
This approach ensures that screening recommendations are tailored to your unique circumstances. Healthcare professionals can also coordinate screening schedules and interpret results in the context of your overall health, providing an integrated approach to managing colorectal health.
Determining the frequency of colorectal cancer screening and the combination of various methods, including lab tests, should be based on a careful evaluation of individual risk factors.



 Lab tests for colon cancer screening
Lab tests for colon cancer screening